Taming Excessive Sweat: Your Guide To Hyperhidrosis Antiperspirants
For millions worldwide, sweating isn't just a natural bodily function; it's a relentless, often embarrassing, and debilitating condition known as hyperhidrosis. This isn't your average perspiration from a workout or a hot day; it's excessive and uncontrollable sweating that can occur regardless of temperature or activity, significantly impacting daily life, social interactions, and even mental well-being. If you find yourself constantly battling damp clothes, clammy hands, or perpetually wet feet, you're not alone, and thankfully, there are effective solutions, with hyperhidrosis antiperspirants often being the first line of defense.
Living with hyperhidrosis can feel like an endless struggle, but understanding the condition and the tools available to manage it is the first step towards reclaiming control. From specialized antiperspirants to advanced medical treatments, a range of options exists to help those affected by this challenging condition. This comprehensive guide will delve deep into the world of hyperhidrosis antiperspirants, exploring how they work, how to choose the right one, and what other treatments are available to help you navigate life with greater comfort and confidence.
Table of Contents
- Understanding Hyperhidrosis: More Than Just Sweat
- The Role of Antiperspirants in Managing Hyperhidrosis
- Choosing the Right Hyperhidrosis Antiperspirant
- Beyond Antiperspirants: Other Management Strategies
- Differentiating Hyperhidrosis from Related Conditions
- When Hyperhidrosis Points to Underlying Health Issues
- Living with Hyperhidrosis: Practical Tips and Support
- Authoritative Insights from Dermatology Experts
Understanding Hyperhidrosis: More Than Just Sweat
At its core, hyperhidrosis is the name given to excessive and uncontrollable sweating. This isn't merely a response to heat or exertion; it's a medical condition where the body produces sweat far beyond what is necessary to regulate body temperature. To understand this, it's helpful to know that sweat is a weak salt solution produced by the eccrine sweat glands, which are found almost everywhere on the body, though they are most concentrated on the palms, soles, and armpits. In individuals with hyperhidrosis, these glands are overactive, often without any clear trigger.
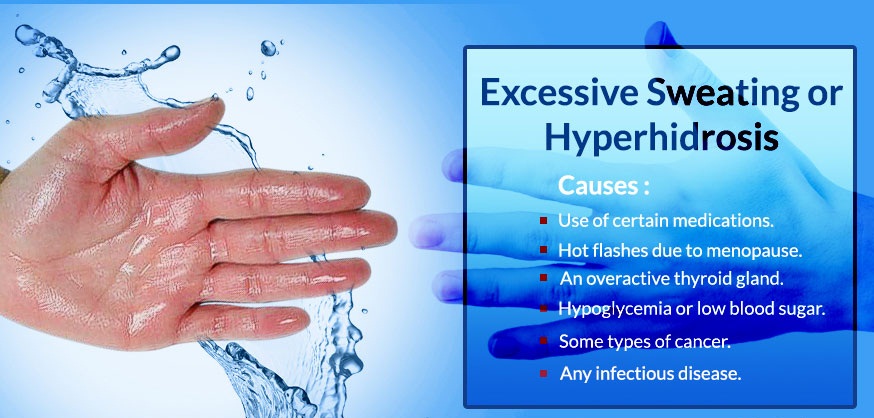
There are two main types of hyperhidrosis: primary focal hyperhidrosis and secondary generalized hyperhidrosis. Primary focal hyperhidrosis typically affects specific areas like the armpits (axillary hyperhidrosis), palms (palmar hyperhidrosis), or soles of the feet (plantar hyperhidrosis), and often begins in childhood or adolescence. It's not usually caused by another medical condition or medication. Secondary generalized hyperhidrosis, on the other hand, is sweating over large areas of the body and is a symptom of an underlying medical condition, such as thyroid problems, diabetes, or certain infections, or a side effect of medication. Understanding which type you might have is crucial for determining the most effective treatment path, but for many, the journey begins with specialized hyperhidrosis antiperspirants.
The Role of Antiperspirants in Managing Hyperhidrosis
When it comes to managing excessive sweating, antiperspirants are often the first line of defense. Unlike deodorants, which merely mask body odor, antiperspirants actively reduce sweat production. They achieve this primarily through their active ingredients, typically aluminum compounds like aluminum chloride or aluminum zirconium. When applied to the skin, these compounds dissolve in sweat and form a temporary plug in the sweat ducts, signaling to the eccrine glands to reduce sweat output. This blockage is superficial and temporary, usually washing away over time, requiring regular reapplication.
While commonly associated with underarm use, typically, antiperspirants are used for axillary hyperhidrosis, but can also be used on other areas prone to hyperhidrosis. This includes areas containing two types of glands, meaning they can be effective on palms, soles, and even the face or back, though formulations may vary for sensitive areas. The effectiveness of an antiperspirant for hyperhidrosis depends largely on the concentration of its active ingredient. Over-the-counter options usually contain lower concentrations, while prescription-strength antiperspirants contain higher percentages of aluminum chloride, offering a more potent solution for severe cases. The key is consistent and correct application, often at night on dry skin, to allow the active ingredients to form effective plugs in the sweat ducts.
Choosing the Right Hyperhidrosis Antiperspirant
Selecting the ideal hyperhidrosis antiperspirant involves understanding the strength of the product and how to apply it for maximum efficacy. For mild to moderate hyperhidrosis, many individuals start with clinical-strength antiperspirants available over-the-counter. These products typically contain higher concentrations of aluminum chloride or aluminum zirconium compared to regular deodorants, often ranging from 15% to 20%. Brands like Certain Dri, Drysol (prescription-strength in some regions), and Odaban are popular choices known for their higher active ingredient content.
If over-the-counter options prove insufficient, a dermatologist might recommend a prescription-strength antiperspirant, which can contain aluminum chloride hexahydrate in concentrations as high as 20% or even more. These are significantly more potent and are often applied once daily at bedtime to clean, completely dry skin. Applying to wet skin can lead to irritation and stinging. The idea is to allow the product to work overnight when sweat glands are less active, and then wash it off in the morning. As sweating decreases, the frequency of application can often be reduced to a few times a week. It's crucial to follow the specific instructions provided by your doctor or on the product packaging to minimize potential side effects like skin irritation, redness, or itching, which are more common with higher concentrations of active ingredients.
Beyond Antiperspirants: Other Management Strategies
While hyperhidrosis antiperspirants are a foundational treatment, they are not the only solution. For those who don't find sufficient relief, or for specific types of hyperhidrosis, several other effective medical interventions are available. These range from in-office procedures to oral medications, each with its own mechanism of action and suitability for different individuals.
Iontophoresis: A Water-Based Solution
Iontophoresis is a popular and effective treatment, particularly for palmar and plantar hyperhidrosis. The process involves submerging the affected areas (typically hands or feet) in a shallow pan of water while a low-level electrical current is passed through the water. This current is believed to temporarily block the sweat ducts, reducing sweat production. Iontophoresis for hyperhidrosis is usually carried out with ordinary tap water, however, sodium chloride electrolyte solution or an anticholinergic agent such as glycopyrronium bromide) can be added to enhance its effectiveness. Sessions typically last 15-20 minutes and are performed several times a week initially, then reduced to a maintenance schedule. While the exact mechanism is not fully understood, it's a safe and non-invasive option for many.
Oral Medications: Targeting the System
For more widespread or severe cases of hyperhidrosis, oral medications may be prescribed. The most common class of drugs used are anticholinergics. These medications work by blocking the action of acetylcholine, a neurotransmitter that signals the sweat glands to produce sweat. Anticholinergic medication, anticholinergics, anticholinergic agent, parasympatholytic drug, acetylcholine receptor antagonist, muscarinic receptor blocker – these are all terms for drugs that interfere with the nervous system's signals to the sweat glands. Drugs can act on the hypothalamus or at spinal levels to reduce overall sweating. While effective, anticholinergics can cause side effects such as dry mouth, blurred vision, constipation, and difficulty urinating, which limit their use for some individuals. Other oral medications, such as beta-blockers or benzodiazepines, might be used in specific situations, particularly if anxiety triggers sweating.
Botulinum Toxin Injections
Botulinum toxin injections, commonly known by brand names like Botox, are an FDA-approved treatment for severe axillary hyperhidrosis and can also be used off-label for palms, soles, and the face. The toxin works by temporarily blocking the nerves that stimulate sweat glands. A series of small injections are administered directly into the affected area. The effects typically last for 4-12 months, after which repeat injections are needed. While effective, the procedure can be uncomfortable, and potential side effects include temporary muscle weakness in the treated area (especially palms) or bruising.
Surgical Options
For very severe and debilitating cases of hyperhidrosis that have not responded to other treatments, surgical interventions may be considered. The most common surgical procedure is endoscopic thoracic sympathectomy (ETS), which involves cutting or clamping the sympathetic nerves that control sweating in specific areas, most commonly the hands. While highly effective for palmar hyperhidrosis, ETS carries the risk of compensatory sweating, where excessive sweating develops in other areas of the body, such as the back or trunk, which can sometimes be more bothersome than the original problem. Other surgical approaches, like local sweat gland removal (curettage or liposuction), are sometimes used for axillary hyperhidrosis.
Differentiating Hyperhidrosis from Related Conditions
It's important to distinguish hyperhidrosis from other sweat-related or skin conditions that might present similarly or be exacerbated by excessive sweating. One common concern is body odor. Bromhidrosis (osmidrosis or ozochrotia) is an unpleasant body odour due to any cause including poor hygiene, infection, diet, or medication. While hyperhidrosis can contribute to bromhidrosis by creating a moist environment conducive to bacterial growth, they are distinct conditions. Addressing bromhidrosis might involve specific antibacterial soaps, topical antibiotics, or dietary changes, in addition to managing the underlying sweat.
Excessive moisture can also lead to or worsen certain skin conditions. For instance, keratolysis exfoliativa is a common skin condition in which there is focal peeling of the palms and less often the soles. It is also known as exfoliative keratolysis. This condition can be exacerbated by constant wetness, leading to a breakdown of the skin's outer layer. Similarly, dyshidrotic eczema (pompholyx) is an itchy, chronic, recurrent, often symmetric eruption on the palms of hands, fingers, and soles of the feet. While the exact cause is unknown, it's often triggered or worsened by sweating, stress, or contact with irritants. Managing hyperhidrosis effectively can play a significant role in improving these related dermatological issues and improving overall skin health.
When Hyperhidrosis Points to Underlying Health Issues
While primary focal hyperhidrosis is a standalone condition, excessive sweating can sometimes be a symptom of a more serious underlying medical problem. This is known as secondary hyperhidrosis. It's crucial to consult a healthcare professional if your sweating is generalized (affecting large areas of the body), starts suddenly, occurs primarily at night, or is accompanied by other symptoms like weight loss, fever, or palpitations. Several conditions can cause secondary hyperhidrosis, including:
- **Endocrine disorders:** Hyperthyroidism (overactive thyroid), diabetes, menopause, and pheochromocytoma.
- **Neurological conditions:** Stroke, Parkinson's disease, and autonomic neuropathy.
- **Infections:** Tuberculosis, endocarditis, and osteomyelitis.
- **Certain cancers:** Lymphoma and other malignancies.
- **Medications:** Some antidepressants, pain medications, and drugs for diabetes or Alzheimer's disease can induce sweating as a side effect. It's important to note that individuals with conditions like cystic fibrosis or cystic fibrosis carriers, Raynaud disease, marasmus (severe form of protein deficiency malnutrition), and atopic dermatitis, or those who take particular medications, may experience hyperhidrosis as a related symptom or side effect.
- **Specific syndromes:** For example, hyperhidrosis in Ross syndrome is a compensatory mechanism usually involving unilateral segments most commonly on the trunk between the T5 and T12 dermatomes. This rare neurological disorder presents with a combination of segmental anhidrosis (lack of sweating) and compensatory hyperhidrosis in other areas.
A thorough medical evaluation, including a review of your medical history, current medications, and possibly blood tests, is essential to rule out any underlying causes before focusing solely on symptomatic treatment with hyperhidrosis antiperspirants or other methods.
Living with Hyperhidrosis: Practical Tips and Support
Beyond medical treatments, several practical strategies can help individuals cope with the daily challenges of hyperhidrosis. These tips focus on managing symptoms and minimizing their impact on your life:
- **Clothing Choices:** Opt for loose-fitting clothing made from natural, breathable fabrics like cotton, linen, or bamboo. Wicking fabrics designed for athletic wear can also be beneficial as they draw moisture away from the skin. Avoid tight clothing and synthetic materials that can trap heat and moisture.
- **Footwear:** Wear shoes made of leather or canvas that allow your feet to breathe. Change socks frequently, especially if they become damp, and choose socks made from moisture-wicking materials. Alternating shoes daily can allow them to dry out completely.
- **Hygiene:** Regular bathing helps control bacteria that contribute to odor. Using antibacterial soaps can also be beneficial.
- **Powders:** Applying absorbent powders (like cornstarch or talc-free body powder) to affected areas can help absorb excess moisture and reduce friction.
- **Carry Essentials:** Keep extra shirts, socks, or a small towel handy if you anticipate sweating.
- **Stress Management:** Stress and anxiety can often trigger or worsen sweating episodes. Practicing relaxation techniques like deep breathing, meditation, or yoga can be helpful.
- **Dietary Considerations:** Some people find that certain foods or drinks, such as spicy foods, caffeine, or alcohol, can exacerbate sweating. Identifying and limiting these triggers might provide some relief.
Living with hyperhidrosis can be emotionally taxing, leading to self-consciousness, social anxiety, and even depression. Seeking support from friends, family, or support groups can be invaluable. Remember, you are not alone, and many resources are available to help you manage this condition effectively.
Authoritative Insights from Dermatology Experts
When dealing with a persistent medical condition like hyperhidrosis, seeking information from reliable and authoritative sources is paramount. Organizations like DermNet New Zealand are excellent resources, providing comprehensive and evidence-based information on various skin conditions, including those related to sweating and sweat glands. Their content is peer-reviewed and regularly updated by dermatologists, ensuring that the facts presented are accurate and trustworthy. For anyone seeking to understand the nuances of hyperhidrosis, its causes, and its treatments, consulting such expert-driven platforms is highly recommended.
Dermatologists are the specialists best equipped to diagnose and manage hyperhidrosis. They can accurately assess your condition, differentiate between primary and secondary hyperhidrosis, and recommend the most appropriate treatment plan tailored to your specific needs. This might involve starting with strong hyperhidrosis antiperspirants, progressing to iontophoresis, oral medications, or injections if necessary. They can also provide guidance on managing side effects and offer insights into newer treatments as they become available. Relying on authoritative facts from DermNet New Zealand and similar medical bodies, alongside professional medical advice, ensures that you receive the best possible care for your condition. Always remember to discuss your symptoms and concerns openly with your doctor to explore all viable options.
Conclusion
Hyperhidrosis, or excessive and uncontrollable sweating, is a challenging condition that affects millions globally, but it is far from untreatable. From the initial step of incorporating specialized hyperhidrosis antiperspirants into your daily routine to exploring advanced medical interventions like iontophoresis, oral medications, or even surgical options, a spectrum of solutions exists to help you regain control and improve your quality of life. Understanding the distinction between primary and secondary hyperhidrosis, and recognizing when excessive sweating might signal an underlying health issue, is crucial for effective management.
By combining effective treatments with practical lifestyle adjustments and seeking guidance from trusted dermatological resources like DermNet New Zealand, individuals with hyperhidrosis can significantly reduce their symptoms and live more comfortably. If you've been silently struggling with excessive sweating, it's time to take action. Consult with a healthcare professional to discuss your options and embark on a path toward drier, more confident days. Don't let hyperhidrosis define you; empower yourself with knowledge and appropriate care. What steps will you take today to manage your hyperhidrosis effectively?


Detail Author:
- Name : Clifton Hahn
- Username : qrunolfsson
- Email : vhintz@gmail.com
- Birthdate : 2005-02-07
- Address : 9962 Bogisich Lights Lake Shaniehaven, SD 95847
- Phone : +1.651.728.3166
- Company : Kemmer and Sons
- Job : Mining Machine Operator
- Bio : Officiis quidem repellat consequuntur. Amet porro repudiandae natus voluptas adipisci est. Perspiciatis cum illo voluptatibus adipisci neque.
Socials
facebook:
- url : https://facebook.com/octavia_dev
- username : octavia_dev
- bio : Voluptas voluptas quis et sunt velit ipsum.
- followers : 2751
- following : 2520
tiktok:
- url : https://tiktok.com/@ohudson
- username : ohudson
- bio : Distinctio ut ut ut ut voluptatem in autem.
- followers : 4362
- following : 2640
instagram:
- url : https://instagram.com/hudson1985
- username : hudson1985
- bio : Hic cupiditate sit ipsam dignissimos vel unde. Laborum labore consequatur atque sequi at eum sunt.
- followers : 980
- following : 1666