Unraveling "DID": Beyond Celebrity Buzz
In the vast ocean of online searches, a curious query occasionally surfaces: "did Rosie O'Donnell move to Ireland?" While the internet often buzzes with celebrity whereabouts, this particular phrasing inadvertently opens a door to a far more profound and vital conversation. The seemingly simple word "did" can, in fact, be an acronym for something entirely different, a complex mental health condition known as Dissociative Identity Disorder. This article will delve deep into the intricacies of DID, shedding light on a condition that, much like the initial search query, is often misunderstood and shrouded in misconception.
Our aim is not to speculate on celebrity residences, but rather to use this common linguistic ambiguity as a starting point to explore a significant and often stigmatized mental health challenge. Dissociative Identity Disorder, or DID, is a condition that impacts individuals in profound ways, yet remains one of the most frequently misconstrued psychiatric disorders. By providing solid research and clear explanations, we hope to foster a greater understanding and reduce the stigma surrounding this complex reality.
- Morgan Lane
- Burns Film Center Movies
- Newnan Times Herald
- Snowbasin Ski Resort
- Crazy Days And Crazy Nights
Table of Contents
- Understanding Dissociative Identity Disorder (DID): A Complex Reality
- The Roots of DID: Trauma and Dissociation
- Recognizing the Symptoms of DID
- The Diagnostic Journey for DID
- Treatment Pathways for DID: Hope and Healing
- The Ongoing Debate and Research in DID
- Living with DID: Challenges and Resilience
- Spreading Awareness and Reducing Stigma
Understanding Dissociative Identity Disorder (DID): A Complex Reality
Dissociative Identity Disorder (DID) is a mental health condition characterized by the presence of two or more distinct identities or personality states. These separate identities alternately take control of an individual, leading to significant disruptions in memory, consciousness, identity, emotion, perception, body representation, motor control, and behavior. It is a rare condition, often misunderstood by the general public and even some professionals, making accurate information crucial.
Historically, DID was known as multiple personality disorder until 1994, when its name was changed to better reflect the understanding that it is not about having "multiple personalities" but rather a fragmentation of one's identity. This distinction is vital for addressing misconceptions and promoting accurate understanding. The condition is deeply complex, affecting an individual's entire experience of self and the world around them. It is one of the most misunderstood psychiatric disorders, frequently sensationalized in media, which further contributes to the stigma surrounding it. Therefore, it’s important to address misconceptions with solid research to spread understanding and reduce the stigma that often prevents individuals from seeking help.
The Roots of DID: Trauma and Dissociation
At the core of Dissociative Identity Disorder lies a profound connection to severe and repetitive trauma, particularly that experienced during early childhood. Research consistently shows that most people with DID have experienced repetitive and severe childhood trauma, including physical and sexual abuse, emotional neglect, and a dysfunctional home environment. This trauma is often pervasive and chronic, occurring at a critical developmental stage when a child's sense of self is still forming.
In response to overwhelming and inescapable trauma, the mind employs a powerful defense mechanism: dissociation. Dissociation is a mental process that causes a lack of connection in a person's thoughts, memories, feelings, actions, or sense of identity. For individuals who develop DID, this dissociation becomes an extreme, involuntary coping strategy. It can be a way for them to escape from negative experiences they’ve lived, essentially creating psychological distance from the unbearable pain and terror of their reality. By compartmentalizing traumatic memories, emotions, and even aspects of their identity, the individual is able to survive otherwise intolerable circumstances. Over time, these dissociated states can develop into distinct identities, each with its own patterns of perceiving, relating to, and thinking about the self and the environment. This profound fragmentation highlights the incredible resilience of the human mind, even as it grapples with immense suffering.
Recognizing the Symptoms of DID
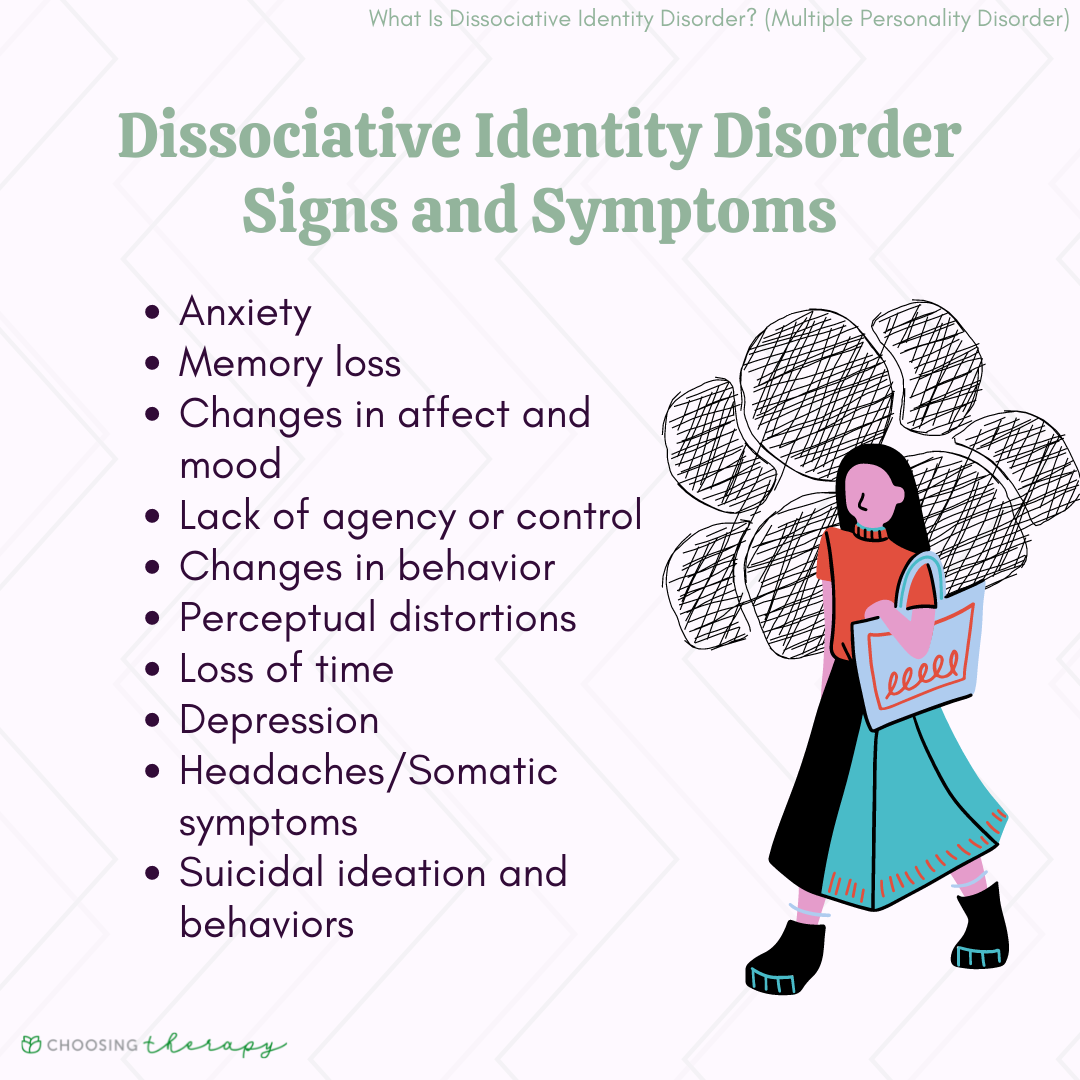
Identifying Dissociative Identity Disorder can be challenging due to its complex and often subtle presentation, as well as its tendency to be confused with other mental health conditions. However, understanding the core symptoms is crucial for proper diagnosis and support. DID is a disorder associated with severe behavioral health symptoms, which can manifest in various ways beyond the hallmark identity shifts.
The Core Symptom: Identity Fragmentation
The most recognizable symptom of Dissociative Identity Disorder (DID) is a person’s identity being involuntarily split between at least two distinct identities (personality states). These "alters," as they are often called, are not just different moods or roles; they are experienced as separate individuals with their own unique names, ages, genders, mannerisms, voices, and even physical characteristics (though the latter is perceived, not actual biological change). These identities alternately take control of the individual's behavior, thoughts, and feelings. This shift can be sudden and dramatic, often accompanied by memory gaps or amnesia regarding the actions and experiences of other identities. For instance, an individual might "wake up" in a different location with no memory of how they got there, or find objects they don't recall purchasing.
Other Behavioral Health Symptoms
Beyond the fragmentation of identity, individuals with DID often experience a range of other severe behavioral health symptoms. These can include:
- **Severe memory loss (amnesia):** Not just forgetting everyday things, but significant gaps in memory for personal information, important events, and daily activities, especially those related to other identities.
- **Depersonalization:** Feeling detached from one's own body, thoughts, feelings, or actions, as if observing them from outside.
- **Derealization:** Feeling that the world around them is unreal, dreamlike, foggy, or distorted.
- **Identity confusion:** A sense of confusion about who they are, their values, or their purpose.
- **Depression and anxiety:** High rates of mood disorders and anxiety disorders are common.
- **Self-harm and suicidal ideation:** A significant risk due to the intense emotional pain and distress associated with the disorder.
- **Eating disorders and substance abuse:** Often used as coping mechanisms.
- **Sleep disturbances:** Including nightmares, night terrors, and insomnia.
- **Flashbacks and intrusive thoughts:** Re-experiencing traumatic events as if they are happening in the present.
DID vs. Other Conditions
DID, associated with early childhood trauma, is largely misunderstood and often confused for other conditions, such as schizophrenia, borderline personality disorder, or even bipolar disorder. This confusion arises because some symptoms, like hearing voices or rapid mood swings, can superficially resemble those of other conditions. However, a key differentiator in DID is the distinct, separate identities and the profound amnesia between them, which is not characteristic of these other disorders. It's important for clinicians to learn to spot the symptoms and understand how it can be treated, avoiding misdiagnosis that can delay appropriate and effective care.
The Diagnostic Journey for DID
The path to a correct diagnosis of Dissociative Identity Disorder can often be long and challenging, primarily due to its complexity and the common misconceptions surrounding it. However, it is crucial to emphasize that DID is a treatable disorder once it is properly diagnosed. The journey begins with a comprehensive and sensitive assessment by mental health professionals who are knowledgeable about dissociative disorders.
Clinicians who understand DID symptoms can diagnose DID in the clinical interview. This involves a thorough exploration of the individual's history, current symptoms, and experiences, paying close attention to signs of identity fragmentation, amnesia, and other dissociative phenomena. The interview process is often extensive, as individuals with DID may not immediately present with overt signs of identity switching, and may even try to conceal their symptoms due to shame or fear. Building trust with the clinician is paramount for accurate assessment.
In addition to clinical interviews, there are also paper and pencil tests that can help in the diagnostic process. These standardized psychological assessments, such as the Dissociative Experiences Scale (DES) or the Structured Clinical Interview for DSM-5 Dissociative Disorders (SCID-D), are designed to identify and measure the presence and severity of dissociative symptoms. While these tests are valuable tools, they are typically used in conjunction with a thorough clinical interview and observation, rather than as standalone diagnostic instruments. A proper diagnosis is the first critical step toward unlocking effective treatment and enabling individuals to begin their journey toward integration and healing.
Treatment Pathways for DID: Hope and Healing
Once Dissociative Identity Disorder is properly diagnosed, the focus shifts to comprehensive treatment, which is typically a long-term process requiring patience, commitment, and a highly specialized therapeutic approach. The primary goal of treatment is to help the individual integrate their fragmented identities into a cohesive sense of self, process the underlying trauma, and develop healthier coping mechanisms. While challenging, DID is a treatable disorder, and many individuals achieve significant improvement and a better quality of life.
The most effective therapeutic approach for DID is typically trauma-informed psychotherapy, often a long-term process of individual therapy. Key therapeutic approaches include:
- Phase-Oriented Treatment: This model typically involves three phases:
- Phase 1: Safety and Stabilization: Focusing on establishing a sense of safety, building coping skills, and managing intense emotional dysregulation and self-harming behaviors. This phase also involves building a trusting therapeutic relationship.
- Phase 2: Trauma Processing: Gradually and carefully processing the traumatic memories and experiences that led to the development of DID. This is done in a controlled and supported environment to prevent re-traumatization. Techniques like Eye Movement Desensitization and Reprocessing (EMDR) may be used, adapted for dissociative clients.
- Phase 3: Integration and Rehabilitation: Working towards the integration of fragmented identities, developing a cohesive sense of self, improving daily functioning, and building healthy relationships. This phase focuses on grief work for lost time and experiences, and developing a future-oriented perspective.
- Dialectical Behavior Therapy (DBT): While not specific to DID, DBT skills, particularly those related to emotion regulation, distress tolerance, and interpersonal effectiveness, can be highly beneficial in managing the severe behavioral health symptoms associated with DID.
- Cognitive Behavioral Therapy (CBT): Elements of CBT can help individuals challenge distorted thoughts and develop more adaptive behaviors.
Medication is generally not a primary treatment for DID itself, but it can be used to manage co-occurring symptoms such as depression, anxiety, or sleep disturbances. The journey of recovery for individuals with DID is a testament to human resilience, demonstrating that with proper diagnosis and consistent, specialized therapeutic support, significant healing and integration are possible.
The Ongoing Debate and Research in DID
Despite significant advancements in understanding and treating Dissociative Identity Disorder, the field is not without its complexities and debates. As noted by sources like [61][19][36], the primary dispute is between those who view DID as a genuine, trauma-based mental health condition and those who question its prevalence or even its existence, sometimes attributing symptoms to iatrogenic (therapist-induced) factors or suggestibility. This ongoing academic and clinical discussion highlights the critical need for continued, rigorous research to solidify understanding and refine diagnostic and treatment protocols.
Advancing understanding through research is paramount. Studies continue to explore the neurological underpinnings of dissociation, the long-term efficacy of various therapeutic interventions, and the specific factors that contribute to the development of DID in individuals exposed to trauma. Research also focuses on improving diagnostic tools and criteria, aiming to make it easier for clinicians to accurately identify DID and differentiate it from other conditions. Furthermore, there's a growing emphasis on understanding the lived experience of individuals with DID, moving beyond purely clinical perspectives to incorporate patient narratives and insights. This ongoing scientific inquiry is vital for overcoming skepticism, improving clinical practice, and ultimately, providing better care for those affected by this complex disorder.
Living with DID: Challenges and Resilience
For individuals diagnosed with Dissociative Identity Disorder, navigating daily life presents unique and often profound challenges. The fragmentation of identity and the accompanying symptoms can significantly impact various aspects of an individual's existence. Learning how this condition affects mental health and daily life is crucial for both those who live with DID and their support networks.
The challenges often include:
- Functional Impairment: Difficulty maintaining employment, stable housing, or consistent relationships due to unpredictable identity shifts, memory gaps, and emotional dysregulation.
- Social Isolation: Fear of judgment, misunderstanding, or the perceived strangeness of their experiences can lead individuals to withdraw from social interactions.
- Legal and Financial Difficulties: Amnesia can lead to missed appointments, unpaid bills, or even legal troubles if actions taken by one identity are unknown to others.
- Co-occurring Conditions: High rates of depression, anxiety, eating disorders, substance abuse, and post-traumatic stress disorder (PTSD) further complicate daily functioning.
- Internal Conflict: The presence of different identities can lead to internal struggles, conflicts over decisions, and a pervasive sense of not being whole.
Despite these immense challenges, individuals living with DID also demonstrate incredible resilience. Many learn to develop internal communication strategies between their identities, engage actively in their therapy, and build robust support systems. Support groups, both online and in-person, can provide a vital sense of community and validation. Developing self-care practices, such as mindfulness, creative expression, and grounding techniques, also plays a significant role in managing symptoms and fostering a sense of stability. The journey is long, but with appropriate support and unwavering determination, individuals with DID can achieve remarkable progress in their healing and lead fulfilling lives.
Spreading Awareness and Reducing Stigma
The journey of understanding Dissociative Identity Disorder extends beyond individual diagnosis and treatment; it encompasses a broader societal responsibility to spread accurate information and dismantle the pervasive stigma. Why education matters cannot be overstated: it’s important to address misconceptions with solid research to spread understanding and reduce the stigma around this condition, which has historically been sensationalized and misrepresented in popular culture.
Misinformation perpetuates harmful stereotypes, making it harder for individuals with DID to seek help, receive compassionate care, and integrate into society. By promoting accurate knowledge about DID's trauma-based origins, its symptoms, and its treatability, we can:
- Encourage Early Intervention: Reducing stigma makes it safer for individuals to disclose their symptoms and seek professional help sooner, which can lead to better outcomes.
- Improve Professional Training: Increased awareness can lead to better training for healthcare providers, ensuring more accurate diagnoses and effective, trauma-informed treatment.
- Foster Empathy and Support: A more informed public is more likely to offer understanding and support to individuals with DID, rather than fear or judgment.
- Advocate for Resources: Greater awareness can translate into increased funding for research, specialized treatment centers, and support services.
The future directions for DID awareness involve continued advocacy, accurate media representation, and accessible educational resources. By working collectively to demystify this complex condition, we can create a more compassionate and informed society where individuals with Dissociative Identity Disorder are met with understanding, hope, and the opportunity for healing.
Conclusion
While the initial query "did Rosie O'Donnell move to Ireland" might have seemed simple, it provided an unexpected gateway into the profound and often misunderstood world of Dissociative Identity Disorder. We've explored how DID, a complex mental health condition, is fundamentally rooted in severe childhood trauma, manifesting as a fragmentation of identity and a sophisticated coping mechanism for unbearable pain. We've delved into its core symptoms, the intricate diagnostic process, and the vital pathways to treatment, emphasizing that DID is a treatable disorder offering hope and healing.
Understanding DID requires moving beyond sensationalism and embracing solid research, compassion, and a commitment to reducing stigma. It's a condition that profoundly impacts daily life, yet also showcases immense human resilience. By spreading accurate information and fostering empathy, we contribute to a world where individuals living with DID can find the understanding and support they desperately need.
If you or someone you know is struggling with symptoms that resonate with Dissociative Identity Disorder, please consider reaching out to a qualified mental health professional specializing in trauma and dissociation. Knowledge is the first step towards healing and acceptance. Share this article to help spread accurate information and contribute to a more informed and compassionate community.
:max_bytes(150000):strip_icc()/VWH_Illustration_Common-Symptoms-of-Dissociative-Identity-Disorder-DID_Sydney-Saporito_Final-212d7e91fc2d4c80a22186af0ccff5c2.jpg)
Detail Author:
- Name : Newton Grimes
- Username : meta.russel
- Email : verlie91@breitenberg.biz
- Birthdate : 1991-08-26
- Address : 79178 Zane Circle Suite 767 Murphyberg, AR 08665
- Phone : (520) 307-1369
- Company : Batz Group
- Job : Industrial Engineering Technician
- Bio : Eaque eos harum odio natus. Enim id velit dignissimos qui quisquam.
Socials
tiktok:
- url : https://tiktok.com/@kmann
- username : kmann
- bio : Laborum officia qui repellat doloremque nam.
- followers : 1337
- following : 1309
instagram:
- url : https://instagram.com/mannk
- username : mannk
- bio : Et culpa dolorem id. Et qui quos minima soluta. Animi perspiciatis culpa aut omnis consequatur.
- followers : 5517
- following : 2128
facebook:
- url : https://facebook.com/karen3538
- username : karen3538
- bio : Aliquam ipsa voluptas sint.
- followers : 2688
- following : 2873