Transient Ischemic Attack (TIA): Your Critical Warning Sign For Brain Health
Understanding a Transient Ischemic Attack, often referred to as a TIA, is absolutely vital for anyone concerned about their brain health. Far from being a minor event, a TIA is a serious warning sign, a brief but urgent message from your body that something is amiss with the blood flow to your brain. It's an experience that, while temporary, demands immediate attention and a comprehensive understanding of its implications.
This "mini-stroke," as it's sometimes called, might last only a few minutes, causing symptoms that quickly disappear. However, the transient nature of these symptoms should not lull anyone into a false sense of security. A TIA signals an increased risk of a full-blown stroke, making prompt evaluation and appropriate medical intervention not just recommended, but absolutely critical for preventing more severe, lasting damage.
Table of Contents
- Understanding Transient Ischemic Attack (TIA): The "Mini-Stroke" Explained
- The Underlying Causes of a Transient Ischemic Attack
- Recognizing the Warning Signs: Symptoms of TIA
- Why Prompt Evaluation is Crucial for TIA
- Diagnosing a Transient Ischemic Attack: A Comprehensive Approach
- Treatment Strategies for Preventing Future Strokes After a TIA
- The Link Between TIA, Stroke, and Vascular Dementia
- Living Beyond a TIA: Support and Recovery
Understanding Transient Ischemic Attack (TIA): The "Mini-Stroke" Explained
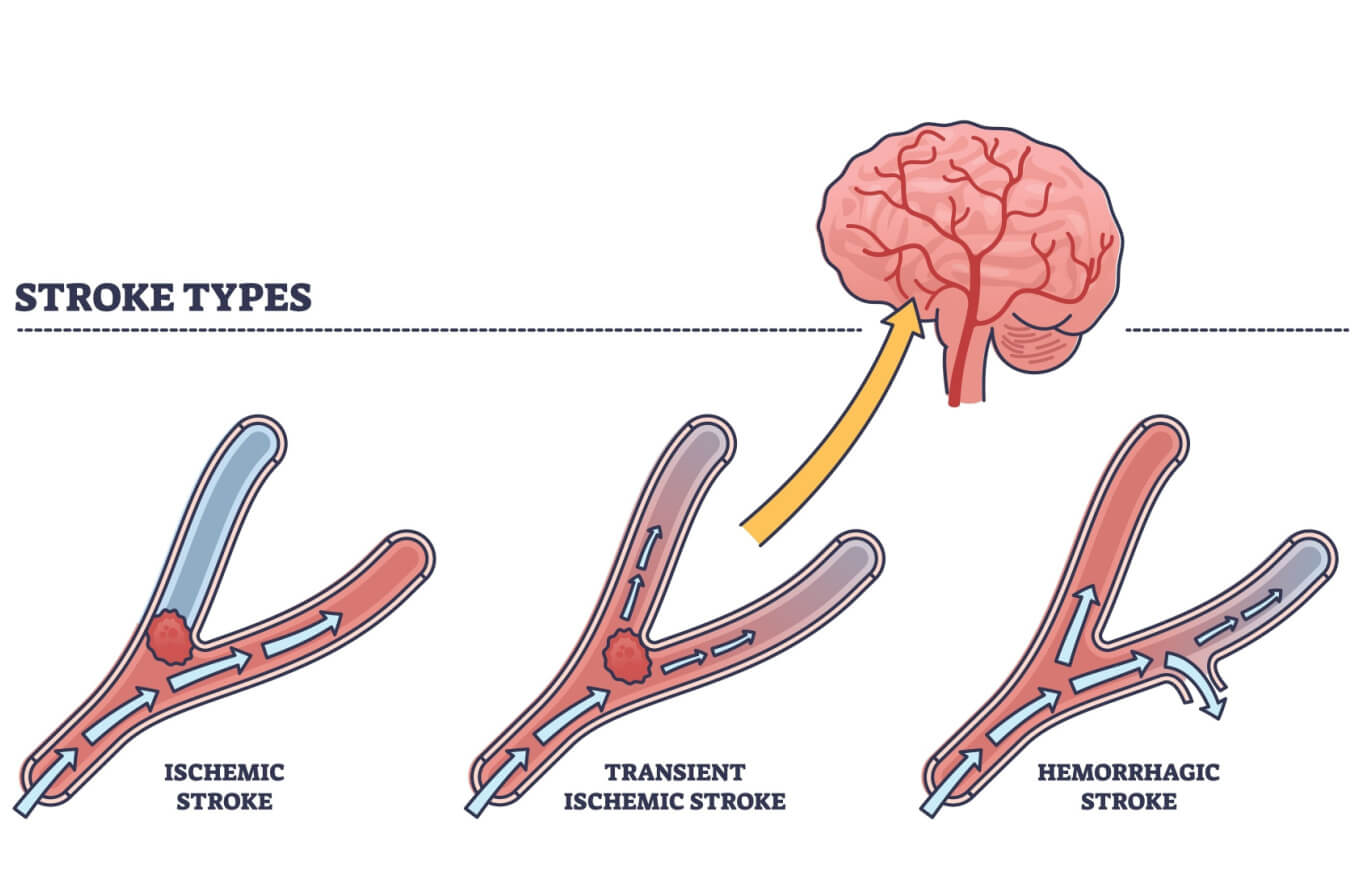
A Transient Ischemic Attack (TIA) is best understood as a temporary disruption of blood flow to a part of the brain, the spinal cord, or the retina (the thin layer of tissue at the back of the eye). This brief blockage causes symptoms that are strikingly similar to those of a stroke, but with a key difference: TIA symptoms typically resolve within a few minutes, and by definition, they do not cause permanent brain damage. This is why it's often informally referred to as a "mini-stroke."
However, the term "mini-stroke" can be misleading if it suggests a minor or insignificant event. On the contrary, a TIA is a potent indicator of an underlying problem with the blood supply to the brain, serving as a critical alarm bell. It signifies that you are at a significantly higher risk of experiencing a full-blown, debilitating stroke in the near future. The prompt and accurate diagnosis of a Transient Ischemic Attack is therefore not just important, but absolutely essential for preventing potentially life-altering consequences.
The Underlying Causes of a Transient Ischemic Attack
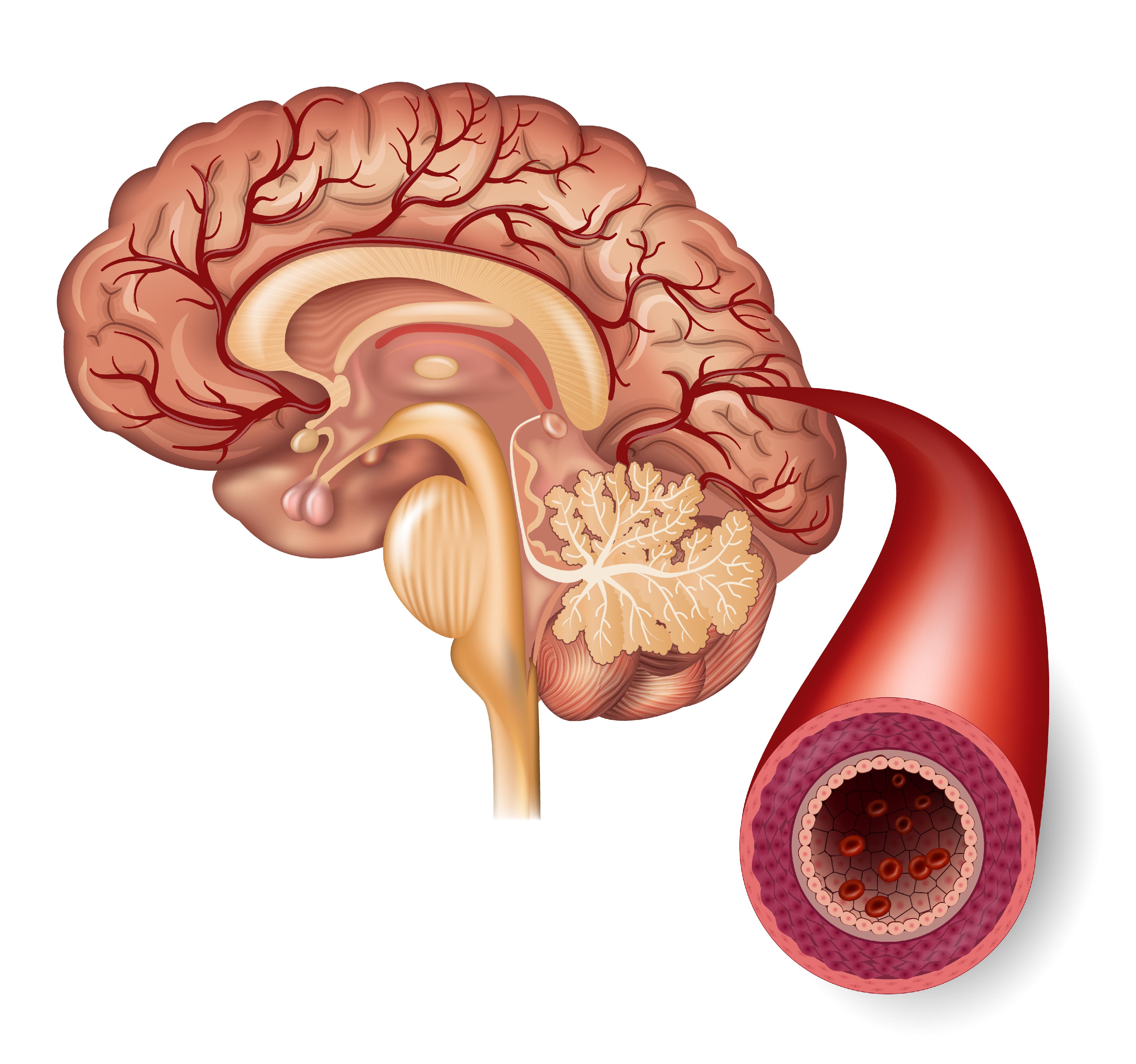
At its core, a Transient Ischemic Attack is caused by a brief, temporary blockage of blood flow. This blockage deprives brain tissue, or sometimes the spinal cord or retina, of the vital oxygen and nutrients it needs to function. Unlike a stroke, where the blockage is prolonged and causes tissue death, in a TIA, the blockage clears quickly, and the symptoms disappear.
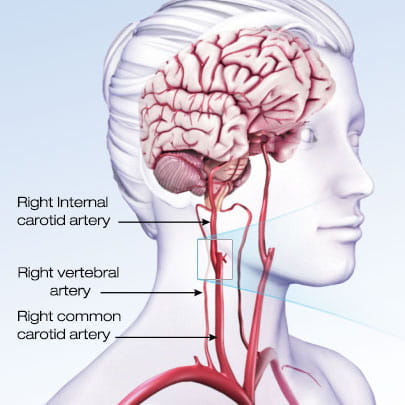
Common Culprits: Carotid Artery Disease and Beyond
One of the most frequent causes of a TIA is carotid artery disease. The carotid arteries are major blood vessels in your neck that supply blood to your brain. Over time, these arteries can become narrowed or hardened due to the buildup of plaque, a condition known as atherosclerosis. This process often develops slowly and silently, with no noticeable symptoms until a significant event occurs. A TIA can be the very first sign that you have carotid artery disease, as a small piece of plaque or a tiny blood clot might break off from the narrowed artery and travel to the brain, temporarily blocking a smaller vessel.
Beyond carotid artery disease, other factors can lead to a Transient Ischemic Attack. These include blood clots that originate in the heart (especially in conditions like atrial fibrillation), other forms of narrowed blood vessels within the brain, or even conditions that make blood more prone to clotting. Understanding the specific cause of your TIA is paramount, as it directly guides the most effective prevention strategies for future, more severe events.
Recognizing the Warning Signs: Symptoms of TIA
The symptoms of a Transient Ischemic Attack are virtually identical to those of a full-blown stroke, making immediate recognition and action crucial. The key differentiating factor is their duration: TIA symptoms are, by definition, temporary, typically lasting only a few minutes, though they can persist for up to 24 hours. Despite their transient nature, these symptoms demand the same urgent response as a stroke.
Common symptoms to watch for include:
- Sudden weakness or numbness: Often affecting one side of the body, such as an arm, leg, or the face.
- Difficulty speaking or understanding speech: Slurred speech (dysarthria) or trouble finding words (aphasia).
- Sudden vision changes: This could be blurred vision, double vision, or even temporary loss of vision in one eye (amaurosis fugax), which is a classic symptom of a TIA affecting the retina.
- Sudden confusion: Difficulty processing thoughts or understanding what's happening.
- Loss of balance or coordination: Sudden dizziness, stumbling, or an inability to walk straight.
- Severe headache: A sudden, severe headache with no known cause.
It's important to remember that even if these symptoms disappear quickly, they are symptoms of a Transient Ischemic Attack and signal an urgent need for medical evaluation. Untreated, a TIA can indeed lead to a stroke, which carries a much higher risk of permanent disability or even death.
Why Prompt Evaluation is Crucial for TIA
The urgency surrounding a Transient Ischemic Attack cannot be overstated. Even though the symptoms might resolve on their own, a TIA is not an event to simply dismiss. A prompt evaluation of your symptoms is absolutely vital to diagnose the underlying cause of a TIA. This immediate assessment is critical not only for identifying what triggered the temporary blockage but also for allowing your healthcare professional to determine the best and most effective treatment plan to prevent a future, potentially devastating stroke.
Think of a TIA as a fire alarm. The smoke may clear, but the alarm ringing indicates a serious risk that needs immediate investigation. Delaying medical attention after a TIA is a dangerous gamble. Studies consistently show that the risk of a full stroke is highest in the hours and days immediately following a TIA. Promptly spotting stroke-like symptoms, even if they are fleeting, leads to faster diagnosis, quicker treatment, and ultimately, less damage to the brain. This proactive approach can literally be the difference between a minor scare and a life-altering disability.
Diagnosing a Transient Ischemic Attack: A Comprehensive Approach
Diagnosing a Transient Ischemic Attack requires a thorough and systematic approach from experienced medical professionals. Since the symptoms are temporary, the diagnosis often relies heavily on the patient's description of what happened, combined with a comprehensive medical evaluation.
Your Mayo Clinic care team, for instance, exemplifies the multidisciplinary expertise needed. Mayo Clinic doctors trained in blood vessel and brain conditions (cerebrovascular specialists) are equipped with the knowledge and resources to accurately diagnose the cause of a TIA. This includes a detailed medical history, a physical and neurological examination, and a battery of diagnostic tests. These tests may include imaging of the brain (like MRI or CT scans) to rule out a stroke or other brain conditions, imaging of the blood vessels (such as carotid ultrasound, MRA, or CTA) to look for blockages or narrowing, and heart tests (like an EKG or echocardiogram) to check for heart conditions that could cause clots. Blood tests are also crucial to check for conditions like high cholesterol, diabetes, or clotting disorders.
The goal of this comprehensive diagnostic process is not just to confirm that a TIA occurred, but more importantly, to pinpoint the exact reason behind the temporary blockage. This precise identification of the cause is the cornerstone for developing an effective prevention strategy, tailored specifically to your individual risk factors and underlying health conditions.
Treatment Strategies for Preventing Future Strokes After a TIA
Once a Transient Ischemic Attack has been diagnosed and its cause identified, the focus shifts immediately to prevention. The primary goal of treatment is to reduce your risk of experiencing a full stroke, which carries far more severe and lasting consequences. Treatment plans are highly individualized, depending on the underlying cause of the TIA.
Lifestyle Modifications and Risk Factor Management
A significant part of preventing future strokes involves managing controllable risk factors through lifestyle changes. This includes adopting a heart-healthy diet rich in fruits, vegetables, and whole grains, and low in saturated fats, trans fats, and cholesterol. Regular physical activity, maintaining a healthy weight, quitting smoking, and limiting alcohol consumption are also crucial. For individuals with conditions like high blood pressure, diabetes, or high cholesterol, strict management of these conditions through medication and lifestyle adjustments is paramount. These lifestyle changes not only reduce the risk of stroke but also contribute to overall cardiovascular health.
Medical Interventions and Medications
Medications play a pivotal role in stroke prevention after a TIA. Antiplatelet drugs, such as aspirin or clopidogrel, are commonly prescribed. These medications work by making blood platelets less sticky, thereby reducing the likelihood of blood clot formation. In some specific cases, particularly if a large artery is severely blocked, your healthcare provider might recommend cilostazol in addition to aspirin or clopidogrel. Anticoagulants, or blood thinners, may be prescribed if the TIA was caused by a blood clot originating in the heart, as they are more effective at preventing such clots.
If the cause of the TIA is a severe narrowing of the carotid artery in the neck, medical personnel might suggest surgical procedures like carotid endarterectomy or carotid angioplasty and stenting. These procedures aim to open or bypass the narrowed artery, restoring proper blood flow to the brain and significantly reducing stroke risk. The decision for such interventions is made after careful consideration of the individual's overall health, the degree of narrowing, and the specific risks and benefits.
The Link Between TIA, Stroke, and Vascular Dementia
The implications of a Transient Ischemic Attack extend beyond the immediate risk of a stroke. A TIA serves as a powerful indicator of underlying vascular issues that can have long-term consequences for brain health, including the development of vascular dementia. Understanding these connections is essential for comprehensive preventative care.
Understanding the Progression: From TIA to Stroke
A TIA is often described as a "warning stroke" because it signals that the conditions for a full-blown stroke are present. While a TIA's symptoms are temporary and don't cause permanent damage, the underlying problem – a temporary shortage of blood flow – is the same mechanism that causes a stroke. The difference lies in the duration and severity of the blockage. Without intervention, many individuals who experience a TIA will go on to have a stroke, often within days, weeks, or months. This progression underscores the critical importance of treating a TIA as a medical emergency and initiating preventative measures immediately.
The Impact of Vascular Health on Cognitive Function
Beyond acute stroke risk, poor vascular health, as evidenced by a TIA, can also contribute to vascular dementia. Vascular dementia results from conditions that damage your brain's blood vessels, reducing their ability to supply your brain with the amounts of nutrition and oxygen it needs to function properly. This damage can be caused by a series of small, silent strokes (which may or may not cause noticeable TIA-like symptoms) or by widespread damage to the brain's tiny blood vessels. Symptoms of vascular dementia can include difficulties with reasoning, planning, judgment, memory, and other thought processes. Managing the same risk factors that contribute to TIA and stroke—such as high blood pressure, diabetes, and high cholesterol—is therefore crucial for preserving cognitive function and preventing vascular dementia.
Living Beyond a TIA: Support and Recovery
Experiencing a Transient Ischemic Attack can be a frightening and unsettling event. Beyond the immediate medical treatment, living with the aftermath involves ongoing management, vigilance, and often, emotional adjustment. It's a journey that benefits immensely from support and shared experiences.
Connecting with others who have gone through similar experiences can be incredibly valuable. Patient communities, such as Mayo Clinic Connect, offer a platform for individuals living with a TIA to connect with others, share their stories, ask questions, and find support. This sense of community can help alleviate anxiety, provide practical tips for daily living, and offer encouragement during what can be a challenging time.
Long-term management after a TIA involves consistent follow-up with your healthcare team. This ensures that your medications are optimized, your risk factors remain controlled, and any new symptoms are promptly addressed. Regular check-ups, adherence to prescribed treatments, and continued commitment to a healthy lifestyle are cornerstones of preventing future vascular events. Education about your condition, understanding your medications, and knowing the warning signs of a stroke are empowering steps in your recovery journey. By taking an active role in your health, you can significantly reduce your risk and improve your quality of life after a Transient Ischemic Attack.
Conclusion
A Transient Ischemic Attack (TIA) is far more than a fleeting moment of symptoms; it is a critical, urgent warning from your body about the health of your brain's blood supply. While the symptoms may be brief, the underlying causes, often related to conditions like carotid artery disease or blood clots, demand immediate and thorough medical evaluation. Recognizing the symptoms—which mirror those of a stroke—and seeking prompt professional help are paramount to diagnosing the cause and initiating effective preventative treatments.
From lifestyle modifications and essential medications like aspirin or clopidogrel to potential surgical interventions, the goal is always to prevent the progression to a full, debilitating stroke. Furthermore, understanding the profound link between TIA, stroke, and conditions like vascular dementia underscores the long-term importance of managing your vascular health. If you or someone you know experiences symptoms of a TIA, do not hesitate. Act fast, seek medical attention immediately, and engage with your healthcare team to develop a comprehensive plan. Your proactive steps today can safeguard your brain health for tomorrow. Share this vital information with your loved ones, and consider connecting with patient communities for ongoing support and insights.
Detail Author:
- Name : Hillary Kiehn
- Username : yhudson
- Email : ywhite@yahoo.com
- Birthdate : 1972-10-23
- Address : 325 Malika Orchard Brakusmouth, TN 27865-3620
- Phone : 1-458-270-3719
- Company : Dare-Schultz
- Job : Library Assistant
- Bio : Porro et culpa enim tempore ad. Delectus sit sed consectetur perferendis temporibus iure dolorem.
Socials
twitter:
- url : https://twitter.com/egleason
- username : egleason
- bio : Et velit culpa sed repellendus rerum. Voluptatum exercitationem animi enim sunt laudantium ab omnis repellat. Repellat minus velit quisquam accusamus sed.
- followers : 590
- following : 2238
facebook:
- url : https://facebook.com/earlinegleason
- username : earlinegleason
- bio : Tenetur voluptatum quam velit explicabo numquam aliquid error.
- followers : 6795
- following : 2207
linkedin:
- url : https://linkedin.com/in/egleason
- username : egleason
- bio : Velit qui et nihil.
- followers : 4375
- following : 2145